As a result of sweating, heat stress can cause the body to lose a relatively great amount of fluid and electrolytes. This fluid loss can lead to dehydration (lack of water in the body) and may also entail diminished viscosity of the blood. These phenomena increase the risk of thromboses and other cardio-vascular conditions. When thermoregulation (the mechanism of the human body for maintaining a constant body temperature of approx. 37 °C) is restricted, this can bring about disorders in the human water and electrolyte balance which may result in life-threatening impairments of the cardio-vascular system. Groups of individuals particularly at risk include very elderly and sick people, small children and individuals living alone, who cannot ensure – or can only in a limited way ensure – that their body has adequate fluid balance. In extreme cases, heat or rather overheating, can lead to the death of the individual concerned.
Environmental factors also have an influence on health threats from heat. There is evidence from studies that in densely built-up urban areas, where heat islands develop (cf. Indicator BAU-I-2) and where increased values of dust from fine particles and ozone concentrations (cf. Indicator GE-I-9) occur, health risks will increase.
In mortality statistics, mortalities related to heat effects are typically attributed to other causes of death (for instance conditions of the cardio-vascular system). If the amount of mortalities exceeds the seasonally typical and thus expected values, this is taken as an indication that there are extraordinary events involved. The number of heat-related mortalities – in the model underlying the indicator – is estimated as the difference between the modelled mortality and a hypothetical mortality regime. The latter would occur, if the mean weekly temperature (calculated from all hourly values within one week) were not to rise above a fixed temperature threshold, above which the temperature would have a significant effect on mortality. Subject to the age group and region examined, this value would be around 20 °C. Within a range of between 10 °C and 20 °C of a weekly mean temperature, mortality is relatively constant, whereas at a weekly mean temperature of more than 20 °C, it rises distinctly. In weeks with a mean temperature of more than 20 °C there will typically be at least one entire hot day14. Furthermore, the model – which has been developed since the publication of the previous monitoring report – takes into account that also any preceding hot weeks can influence mortality. This is why the mean temperatures of up to three preceding weeks are taken into account. This approach allows identifying any delayed heat effects thus making it possible to convey a clearer picture of the progress of mortality in Germany.
The age group of 85-year old people is most affected by heat-related mortalities in Germany. The analysis of heat-related mortality demonstrates that there are sex-specific differences regarding the number of heat-related mortalities. This is due to the fact that the group comprising people of great age consists of distinctly more women than men. Nevertheless, mortality in all age groups is slightly higher for men than women. This means that within the age groups studied, men succumb to heat impacts more frequently than women. However, overall, more women die from heat-related causes, simply because heat-related mortalities occur most frequently in the group comprising people of great age, as it contains significantly more women.
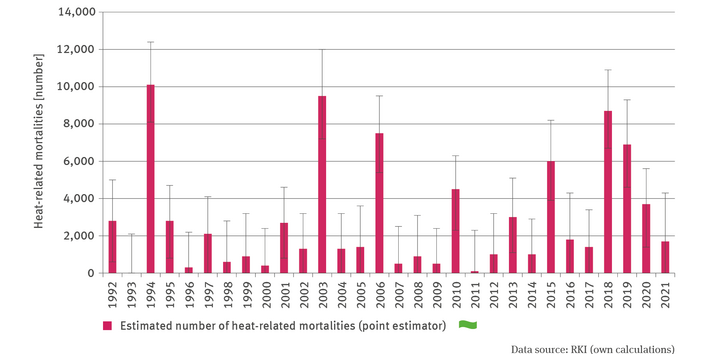
As expected, the time series for heat-related mortalities indicates distinct fluctuations from year to year. This is due to the fact that stronger or weaker heat periods occur in different years in different frequencies and intensities. 2018 was a year characterised throughout Germany by one of the longest heat periods which extended from the whole of July to the whole of August. Moreover, very high weekly mean temperatures were measured during this heat period15. Although some very high temperatures were measured also in 2019, there were repeatedly weeks with lower temperatures interspersed between heat periods. In 2020 the comparatively long heatwave was less hot than in the record summer of 2018, and 2021 was in general a much cooler year.
In the past three decades, a slight decrease in the effect of high temperatures on mortality figures has been observed. To put it briefly: Despite the raised temperatures and the extreme heatwaves, there were – also in summer 2018 – fewer heat-related mortalities than in summer 2003. Presumably, this is because people in Germany have since learned how to cope better with recurring heat periods. Adaptation measures taken by the public health services are likely to have contributed to this positive development. In 2003, the heatwave in Germany hit a relatively ill-prepared country. By comparison, the heat warning service was in operation by 2018 (cf. Indicator GE-R-1), und vorsorgende Maßnahmen waren in vielen stationären Pflegeeinrichtungen etabliert.
Notwithstanding all adaptation measures taken, it has to be said that heat continues to be a serious threat to human health in Germany. It is estimated that in the years from 2018 to 2020 alone, 19,300 individuals succumbed to extreme heat. The focus on potential heat victims will therefore have to be further sharpened, and that means paying particular attention to this issue when drawing up municipal heat action plans.
14 - Winklmayr C., Muthers S., Niemann H., Mücke H.G., an der Heiden M. 2022: Heat-related mortality in Germany from 1992 to 2021. Dtsch Arztebl Int, 119: 451–7. doi: 10.3238/arztebl.m2022.0202
15 - Deutschlandwetter im Sommer 2018: https://www.dwd.de/DE/presse/pressemitteilungen/DE/2018/20180830_deutschlandwetter_sommer_news.html